
If you would like to learn more about the IAEA’s work, sign up for our weekly updates containing our most important news, multimedia and more.
Radiation Therapy on the Wave of Innovation
Eleonora Colzani
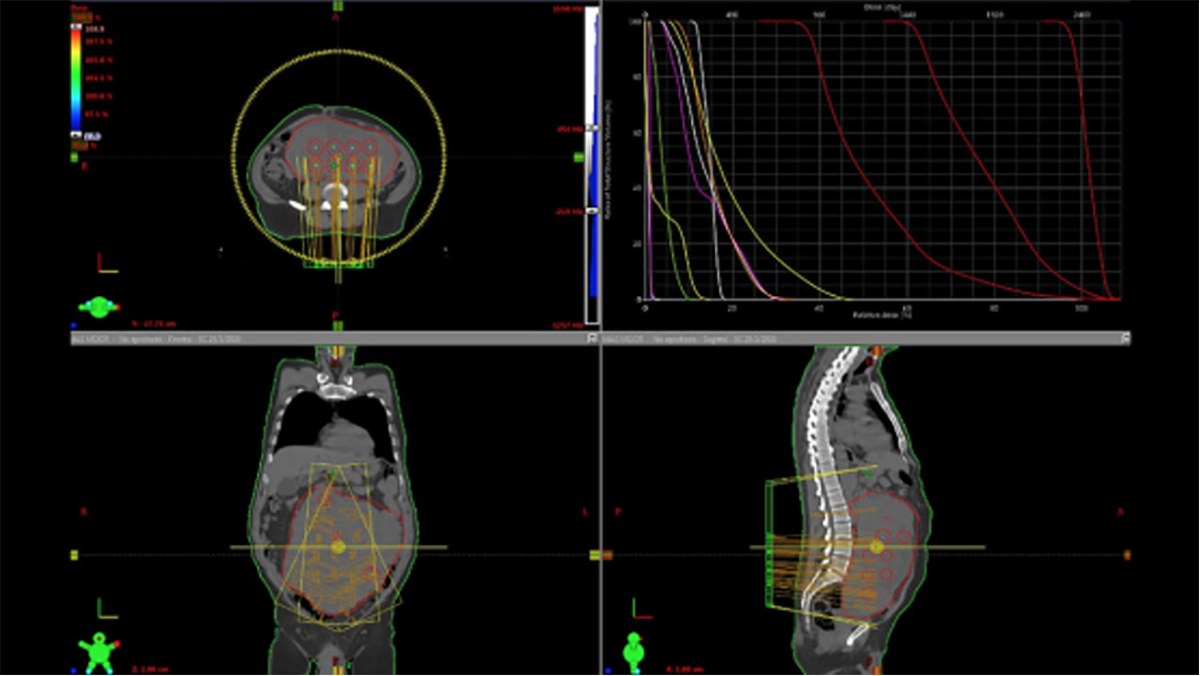
This figure illustrates a large abdominal-pelvic metastatic tumour being irradiated using SFRT. The red ‘bubbles’ represent high radiation doses which directly kill the tumour cells. The areas around the red bubbles in the wider red circle are impacted by lower doses, which provoke an immunological response that further destroys the tumour. (Image: Naipy Perez/Innovative Cancer Institute, USA)
Cancer has always been a concern for humanity. The disease is evident in fossils and mummies, present in historical writings, and can be passed down from our ancestors. In fact, the oldest recorded cases of cancer date back over 3500 years to ancient Egypt, and a malignant tumour has been found on a toe bone of a human fossil that is 1.7 million years old. Today, scientists are developing new forms of cancer treatment such as radiation therapy, also known as radiotherapy, to combat this disease. Radiotherapy involves delivering ionizing radiation from beam generators or radioactive sources to target and destroy cancer cells. In order to reduce the risk of damaging the healthy surrounding tissue, new techniques are being developed to improve the precision of radiotherapy. Riding on the 21st century’s wave of technological innovation, tools and techniques such as stereotactic body radiation therapy, spatially fractionated radiation therapy and artificial intelligence are making treatments more effective and efficient with less side effects.
Stereotactic body radiation therapy
Stereotactic body radiation therapy (SBRT) is an emerging advanced treatment technique that targets tumours with high precision and very high doses of radiation. This delivery method limits the impact on the healthy surrounding tissue, which reduces the likelihood of side effects. As such, it offers a potentially curative therapy or a valuable alternative therapy for many tumour types, including cases in the lungs, liver, brain and pancreas. The IAEA is helping to implement this treatment technique in several countries through coordinated research projects (CRPs) and technical cooperation projects. One such project is devoted to investigating SBRT’s effectiveness in cases of non-operable hepatocellular carcinoma — the most common type of liver cancer and the sixth most common cancer type. “We expect the results of this project will have an impact on current treatment standards and will be particularly relevant for developing countries,” said Lisbeth Cordero, a radiation oncologist at the IAEA involved in the SBRT projects.
Spatially fractionated radiation therapy
Spatially fractionated radiation therapy (SFRT) is a radiotherapy technique that allows for the delivery of relatively high, but varying, doses of radiation across a large tumour, while protecting the healthy surrounding organs. One SFRT technique, grid radiotherapy, uses a physical block with small holes that allows a tumour to receive a combination of high and low doses of radiation. Another technique, lattice radiotherapy, achieves a similar effect using a computer model. “Research suggests an excellent response rate when SFRT is applied to large tumours,” said Cordero. “While SFRT has been used for some time, technological advances now allow for much safer application of such radiotherapy techniques.” In April 2020, the IAEA initiated a CRP on the efficacy of SFRT in the palliative treatment of lung and cervical cancers. The project is investigating the use of SFRT in improving patients’ response to palliative radiotherapy — a treatment that relieves the patients’ symptoms and delays the progression of the disease.
Artificial Intelligence in radiation therapy
Another significant example of how radiation therapy is becoming increasingly innovative is in the application of artificial intelligence (AI). Tools using AI have the power to improve the efficiency, accuracy and quality assurance of radiation therapy. Such tools can be applied at all stages of a patient’s treatment, from diagnosis to treatment and follow-up, bringing about unprecedented improvements in automatization. “In health care, AI is already making its entrance in a variety of subfields, including disease detection. That includes both medical imaging as well as digital pathology, and the optimization of health care services logistics and cancer treatments,” said Jan Seuntjens, Head of Medical Physics at the Princess Margaret Cancer Centre in Canada. The path to the clinical implementation of AI tools is not clear of obstacles, said Kamal Akbarov, a radiation oncologist at the IAEA. He explained that several challenges still lie ahead, leaving many AI tools at a proof-ofconcept stage and far from clinical adoption. Nonetheless, current studies and the increased interest of commercial vendors show the potential of AI tools in radiation therapy. The IAEA held a meeting of experts in October 2021 to discuss AI-based approaches in nuclear technologies, including radiotherapy. Furthermore, a joint project between the IAEA and the European Society for Radiotherapy and Oncology (ESTRO) on radiotherapy contouring skills in AI-enabled clinical environments is planned to start in 2022. The project will consider whether AI can help redistribute the workload from the health workforce by enabling quicker treatment planning.




